Right Bundle Branch Block
What is right bundle branch block?
Right bundle branch block comes from a problem with the heart’s ability to conduct electrical signals. It usually doesn’t cause symptoms unless you have some other heart condition.
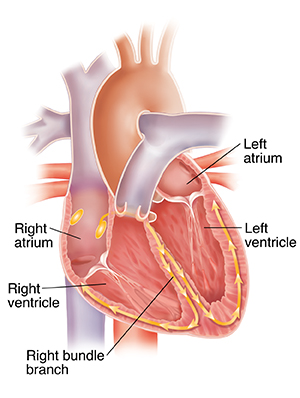
Your heart has 4 chambers. The 2 upper chambers are called atria. The 2 lower chambers are called ventricles. In a healthy heart, the electrical signal for your heartbeat starts in the sinoatrial (SA) node. The SA node is found in the right atrium, the upper right chamber of the heart. From there, the signal is carried to the left atrium and travels to the lower chambers (the right and left ventricles) of the heart. As the signal travels, it triggers nearby parts of the heart muscle to contract in a coordinated manner.
Two special groups of fibers called bundle branches carry the signal from just below the AV node (the junction between the top and bottom chambers of the heart) through the ventricles (bottom of the heart). These are termed right bundle branch and left bundle branch. In right bundle branch block, there is a problem with the right branch of the conducting system that sends the electrical signal to the right ventricle. The electrical signal can’t travel down this path the way it normally would. The signal still gets to the right ventricle, but it has to travel to the left side before getting to the right ventricle. This takes more time. Because of this, the right ventricle contracts a little later than it normally would. This can cause the heart to eject slightly less blood.
Right bundle branch block is rare in healthy young people. It happens more often in older people. This may be due to the normal changes in the heart's conduction system that occurs with age. Right bundle branch block can also occur in people who have another underlying heart or lung problem. It may also be caused as a result of a heart procedure.
What causes right bundle branch block?
Right bundle branch block can result from a number of conditions, such as:
-
Heart disease due to high blood pressure in the lungs (pulmonary hypertension)
-
Chronic obstructive lung disease (COPD)
-
Blood clot in the lung (pulmonary embolism)
-
Right-sided heart failure (cor pulmonale)
-
Disease of the heart muscle (cardiomyopathy)
-
Inflammation of a membrane surrounding the heart (myocarditis)
-
Heart attack
-
Congenital heart disease
-
Inherited arrhythmia syndromes (pseudo right bundle branch block)
-
Interventional or surgical procedures on the heart
All of these conditions increase the risk for right bundle branch block. Sometimes, though, right bundle branch block occurs on its own. The heart may be structurally normal. Researchers aren’t sure what causes these cases of right bundle branch block. In people who have a structurally normal heart, a right bundle branch block is typically not concerning.
Sometimes, right bundle branch block develops after certain procedures. For example, it might develop temporarily during right heart catheter insertion.
What are the symptoms of right bundle branch block?
Usually, right bundle branch block by itself does not cause symptoms. Rarely, right bundle branch block may make symptoms worse in some people with heart failure. Symptoms are more likely to occur if you have other problems in addition to your right bundle branch block.
How is right bundle branch block diagnosed?
Your healthcare provider can diagnose right bundle branch block with the help of an electrocardiogram (ECG). This test provides information about the heart's electrical system. People often first find out they have right bundle branch block when having an ECG done for some other reason. A general practitioner or a cardiologist might first diagnose you.
Your healthcare provider might want to check you for other medical conditions. This includes a thorough history and physical exam. In addition to the ECG, this evaluation might also include the following tests:
How is right bundle branch block treated?
In healthy people without apparent heart disease, right bundle branch block does not appear to have a significant effect on mortality. You may not need any treatment at all for right bundle branch block. People without any symptoms do, however, need careful evaluation at the time of diagnosis.
In people with known or suspected heart disease, right bundle branch block is associated with a greater risk of death, especially after a heart attack.
Some people with right bundle branch block may ultimately need a permanent pacemaker, but this is rare. It is usually only necessary when a person has another conduction problem and right bundle branch block.
How do I manage right bundle branch block?
Your healthcare provider may give you additional instructions about how to manage your right bundle branch block and overall heart health. You might need to make lifestyle changes such as losing weight, quitting smoking, or eating a healthier diet. You'll likely also need to:
-
Monitor your symptoms carefully. Make sure you see a healthcare provider regularly, even if you don’t have any symptoms.
-
Make sure all your healthcare providers know about your right bundle branch block.
When should I call my healthcare provider?
See a healthcare provider right away if you have severe symptoms like chest pain, syncope (fainting), or severe shortness of breath. If you have any new symptoms, plan to see your healthcare provider as soon as possible.
Key points about right bundle branch block
-
Right bundle branch block affects the heart’s conducting system. The right branch of this conducting system is blocked or partially blocked. This causes the right ventricle to contract a little later than it should.
-
Follow your healthcare provider's instructions carefully. Take all your medicines as prescribed.
-
If you have right bundle branch block, see your healthcare provider for follow-up monitoring as advised. This is important even if you don’t have any symptoms.
-
You may need treatment for other health conditions.
-
Most people with right bundle branch block may not require treatment, but some people may eventually need a pacemaker.
-
Tell your healthcare provider if you have severe symptoms or if your symptoms get worse.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is advised and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your provider if you have questions.